
I have had a break from blogging for almost a year now. But I wanted to re-publish this page to continue the work I started on spreading awareness and acceptance for girls on the Autistic Spectrum.
I’ve written for the charity ‘Family Fund’ several times over the past 3 years, since finding out about the wonderful support they offer families who have children with additional needs.
I just wanted to share my friend’s story about her daughter Ruby-Rose who is 16 months old.
On Saturday 13th October 2018, my friend contacted me to say that she’d received a letter stating that Ruby-Rose does not meet the criteria for a Family Fund Grant. In the summer of 2018, after seeing Ruby-Rose several times I encouraged her family to apply for a grant after receiving 3 years of grants that had significantly made a difference for my eldest daughter, Amber (now 6.)
Since the age of 3 months, Ruby’s mother, Claire has been asking my advice as she noticed something regarding Ruby’s development, some may say that this is very young, but I can completely relate as parents, we are the experts on our own children.
Ruby has been seen by a great deal of professionals at her young age, she also received hospital care for Meningitis at 5 months old, this was an extremely worrying time for the whole family. Ruby has been seen by Health Visitors, GPs, Paediatrician, Physioterapist, Specialist Play, and staff at a local SEND school who are offering support as Ruby will need to attend this school when she teaches Nursery/Reception age.
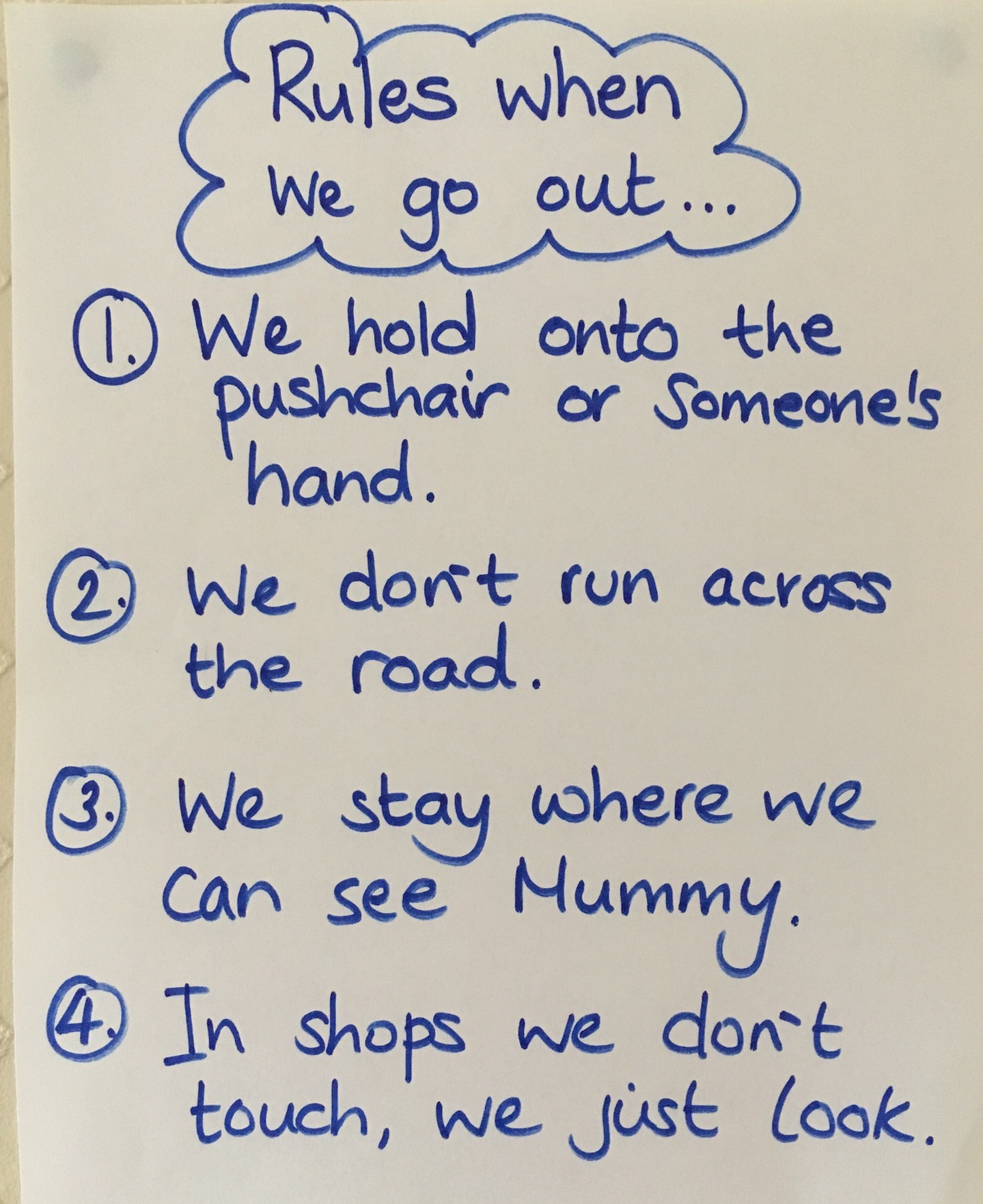
Ruby has been assessed as having a cognitive age of 3 month old, she does not interact with her 2 sisters, to this I’ve witnessed on several occasions. She doesn’t respond to her name and has a great deal of sensory processing difficulties. On the whole, Ruby is a ‘Sensory Avoider’ she is startled by sudden movement, loud and unexpected sounds, has difficulty eating foods that aren’t soft/puréed and therefore has a very restricted diet. She is very tactile defendant, she doesn’t like physical contact and gets distressed, especially when being examined by professionals, such as a Physiotherapist, making it difficult to work with her.
Ruby is currently screams for hours on end and demands and needs around the clock care, she is also having sleep difficulties, finding it hard to settle at night.
Ruby is calmed via sensory equipment such as lights, we known this from when the family attend the ‘stay-and-play’ sessions at the local SEND school and they’ve also taken her to an ‘Autism and Additional Needs’ stay and play session locally. The huge barrier for Ruby’s family, is that the specialist equipment and toys she so desperately needs are very expensive, as you are well aware.
Ruby does not play with regular toys, as ‘Neurotypical’ children her age would, as they are not age appropriate due to her Global Developmental Delay (GDD.)
Ruby requires a calming space she can relax in when she becomes overwhelmed and goes into sensory meltdown. A place where her parents know she will be safe with toys she can not put in her mouth and hurt herself with.
As Ruby hates physical contact, her parents can not hold her to calm her, she doesn’t give eye contact and becomes distressed when doing day to day tasks with her such as feeding and changing her. As she does not sleep through the night, she will sleep for 15-30 minutes and wake up distressed, screaming headbanging to the point she is sick.
Claire, Ruby’s mum, can not work due to Rubys complex needs, and this why the family are struggling financially. All they want is to provide their daughter with the specialist toys and equipment that she desperately needs.
I’ve always been a huge advocate for the work that Family Fund have done for families, I’ve shared this via the parents support group I coordinate locally, to which Ruby’s mother is a member. My own family have had our photographs taken to use for Family Fund promotional materials.
Mum heart is literally breaking for this little girl and her family, I urge you to please re-consider your decision.
Thank you,
Nicki Perrins,
Mum to Amber and Maisie,
Blogger At http://www.spectrumgirls2.com
and coordinator of the Pershore Additional Needs Support group (PANS.)




































You must be logged in to post a comment.